Congressional Briefing Demonstrates the Value of the Medicare Hospice Benefit
New Research Shows Hospice Produces Better Outcomes, Lower Medicare Costs
For Immediate Release
July 28, 2023
(Washington, D.C. and Alexandria, VA) – On Thursday, July 27 a panel of healthcare experts presented groundbreaking new research at a Capitol Hill briefing for Congressional offices, showing that patient use of hospice contributed to $3.5 billion in Medicare savings in 2019, while also providing multiple benefits to patients, families, and caregivers.
The study, conducted by NORC at the University of Chicago, is one of the most comprehensive analyses of enrollment and administrative claims data for Medicare patients covered by Medicare Advantage and Traditional Medicare. The study was funded by the National Association for Home Care & Hospice (NAHC) and the National Hospice and Palliative Care Organization (NHPCO).
Panelists Dianne Munevar, VP of Health Care Strategy at NORC; Dr. Joseph Shega, Chief Medical Office at Vitas; and Susan Lloyd, CEO of Delaware Hospice, related their vast experience with hospice care, extolling its benefit for patients and their loved ones, and also shared findings which prove that longer hospice stays equate to greater savings for taxpayers and overall, better experiences for patients.
Susan Lloyd, CEO of Delaware Hospice shared her personal experience with her mother’s end of life care. “The full benefits of hospice care are realized when the patient and family have the opportunity to engage with the team who provides the support needed wherever [the patient] calls home. Hospice is not a place, it’s a way of caring for people and their loved ones as they are nearing the end of life,” said Lloyd. “One of the greatest blessings of my life was to be there when my mom died. She was not alone; she was surrounded by love. Hospice made that happen for mom, for me, and my family.”
“There’s a lot of myths and misperceptions about what hospice is and what hospice does because of short stays,” said Dr. Joseph Shega, Chief Medical Officer of VITAS. “So when you have a short stay, the hospice does incredible work to try to meet [patients] where they are to honor their wishes […] but if somebody would have that conversation four, five, six, months earlier, they could have an experience like what Jimmy Carter is experiencing now, where he’s chosen he wants to be at home and there’s no difference in life expectancy between those who enroll in hospice earlier vs. those who don’t. With hospice, you can provide that care at home.”
Key findings from the Value of Hospice study include the following:
- NORC estimates that Medicare spending for those who received hospice care was $3.5 billion less than it would have been had they not received hospice care.
- In the last year of life, the total costs of care to Medicare for beneficiaries who used hospice was 3.1 percent lower than for beneficiaries who did not use hospice.
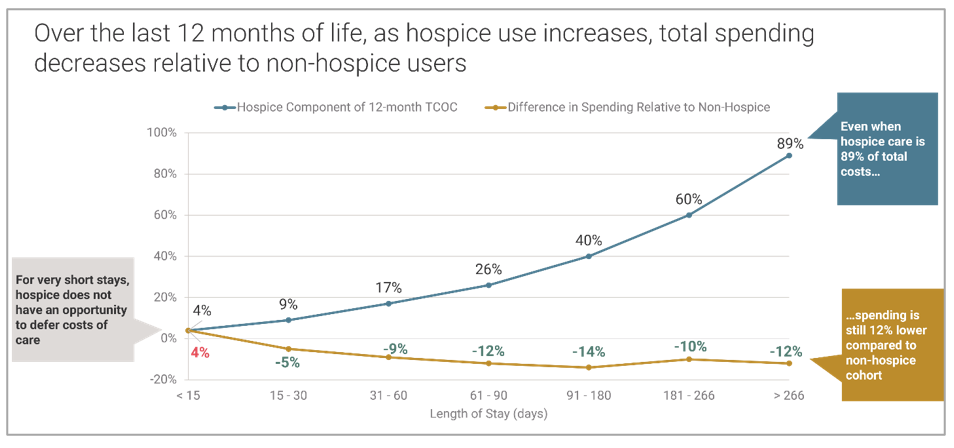
- Hospice is associated with lower Medicare end-of-life expenditures when hospice lengths of stay are 11 days or longer. In other words, earlier enrollment in hospice reduces Medicare spending even further.
- Hospice stays of six months or more result savings for Medicare. For those who spent at least six months in hospice in the last year of their lives, spending was on average 11 percent lower than the adjusted spending of beneficiaries who did not use hospice.
- At any length of stay, hospice care benefits patients, family members, and caregivers, including increased satisfaction and quality of life, improved pain control, reduced physical and emotional distress, and reduced prolonged grief and other emotional distress.
(Source: NORC at the University of Chicago)
“The longer the hospice stay, the more the potential savings,” said Dianne Munevar, Vice President of Health Care Strategy at NORC. “Even when hospice care is 89 percent of total cost, spending is still 12 percent lower compared to the non-hospice [patient]. That’s a huge difference and a huge value to Medicare.” Even when hospice stays exceed six months, Medicare still saves money. “The longer the stay across all disease groups…hospice spending was 11 percent lower than the non-hospice users,” explained Munevar.
A recording of the briefing is available.
###
About NAHC
The National Association for Home Care & Hospice (NAHC) is the voice of home care and hospice. NAHC represents the nation’s 33,000 home care and hospice providers, along with the more than two million nurses, therapists, and aides they employ. These caregivers provide vital services to Americans who are aged, disabled, and ill. Some 12 million patients depend on home care and hospice providers, who depend on NAHC for the best in advocacy, education, and information. NAHC is a nonprofit organization that helps its members maintain the highest standards of care. To learn more, visit nahc.org.
About NHPCO
The National Hospice and Palliative Care Organization (NHPCO) is the nation’s largest and oldest membership association for providers who care for people affected by serious and life-limiting illness. Our members deliver and expand access to high-quality, person-centered interdisciplinary care to millions of Americans. NHPCO provides education and resources to support that mission. Together with our advocacy partner, the Hospice Action Network (HAN), we serve as the leading voice advancing public policy to improve serious-illness and end-of-life care, while our CaringInfo program provides free resources to educate and empower patients and caregivers. nhpco.org
